Should surgical intervention become a primary treatment modality in Crohn’s disease?—A review of the role of surgery and emerging surgical techniques
Naming of Crohn’s disease
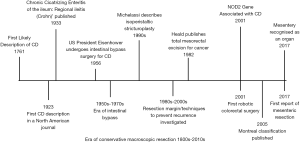
The first description of a disease resembling Crohn’s disease was published in 1761 by Morgagni (Figure 1). He described the post mortem findings of a 20-year-old male, in whom chronic abdominal pain and bloody diarrhea led to death (1). In an article published in 1859 entitled ‘Morbid appearances in the intestine of Miss Bankes’ Wilkes documented macroscopic findings suggestive of Crohn’s disease. He wrote of the terminal ileum in Miss Banke’s case:
‘…. about three feet from its termination in the caecum, the mucous membrane commenced to exhibit an inflammatory response. In the caecum, inflammation of the most acute and violent character was observed ... the bare muscular coat was seen beneath. The muscular coat itself in the caecum was likewise infiltrated with this exudation ... and there is no doubt that through this part of the intestine some transudation had occurred which had set up the peritonitis……’
During the nineteenth century spread of dysentery and diarrheal diseases due to unhygienic living conditions was common. Wilkes presciently suggested idiopathic colitis be considered in a different pathological category to the more common colitides of the time (2). In 1913, Thomas Kennedy Dalziel described ‘hyperplastic enteritis.’ In a series of nine cases, granulomas, eosinophils and giant cells were identified in the intestine, in the absence of an infectious agent such as tuberculosis. Dalziel’s description of the intestine was vivid:
“…. the consistence and smoothness of an eel in a state of rigor mortis….”
In his series, two of the nine cases had stricturing and extensive disease so severe they ultimately succumbed (3). The first description in a North American journal was in 1923. In the American Journal of Medicine, the Mount Sinai pathologist Moschowitz identified ‘nonspecific granulomata’ in intestine that was likely from patients with Crohn’s disease (4).
Burrill B. Crohn, Leon Ginzburg and Gordon Oppenheimer presented a case series of ‘regional ileitis’ at the American Medical Association annual meeting in 1932 (5). At that time, it was journal policy to publish author’s names alphabetically, regardless of manuscript contributions. It is likely this led F.I. Harris to adopt the term ‘Crohn’s disease’ (6). In 1934, the first Crohn’s disease incidence was recorded in Rochester, Minnesota when 1.9 per 100,000 were found to have the disease (7). Colp highlighted the disease’s predilection for the ileocecal region in 1934 (8). In 1937, 5 and 122 cases of regional ileitis were described in England and the US respectively. By 1939, Crohn and colleagues amassed a series of 130 patients (9). In 1943, Tallroth et al. noted a large number of eosinophils in tissue samples from patients with Crohn’s disease, and applied the phrase ‘ileitis allergica’ (10). This association pointed to an immunological factor in either disease aetiology or pathology. In 1952, Charles Wells described regions of healthy bowel between diseased regions (i.e., skip lesions) (11).
Surgical treatment of Crohn’s disease
It became apparent the clinical course of Crohn’s disease is varied and unpredictable. Up to 70% of all patients with Crohn’s disease require surgery with approximately 40% undergoing their first procedure within 10 years of diagnosis. Reoperation rates are also significant (12-17). During Wilke’s era, enteral treatment with copper sulphate, hydrogen peroxide, liver extract, rectal insufflation, artificial fever and, for a short period, abdominal irradiation, were used as treatment modalities (18). The inexorable progression towards the requirement for surgical intervention was soon recognized. Radical intestinal (i.e., longitudinal) resection was first adopted in line with Dalzeil’s suggestion in 1913 (3):
“one does not hesitate in resecting large portions of the intestine”.
In 1941, Crohn strongly recommended surgical excision of diseased tissue saying:
“A specific conservative or medical approach does not exist; the long, slowly downward course cannot be interfered with or changed by any method now known. Vaccines and specific and nonspecific protein therapy have not been of any avail (19).”
In 1941, Wirts identified phenotypes, classifying these according to clinical presentation as: (I) resembling ulcerative colitis; (II) resembling acute appendicitis; (III) with obstructive symptoms; and (IV) with fecal fistula. Patients with more severe disease were treated with extensive resection of all macroscopically diseased intestine. Disease recurrence rates were high, as were rates of short bowel syndrome resulting from extensive and repeated excisions (19).
Intestinal bypass
Intestinal bypass next emerged as a surgical approach in Crohn’s disease (19,20). Bypass relieved ileal obstruction and could be performed expeditiously in unwell patients. It also protected against blow out of the transected ileum. The latter was not uncommon if the intestine was divided proximal to a region of obstruction then returned to the peritoneal cavity (21). In 1956, one month after being diagnosed with regional enteritis, 65-year-old American president Dwight Eisenhower, underwent emergency bypass surgery for Crohn’s disease. He had approximately 35 centimetres affected by a ‘chronic, dry type of regional enteritis’. A double layer ileo-transverse colostomy was created approximately 13 cm proximal the terminal ileum. This approach was greeted with controversy but served Eisenhower well until in 1969, when he was urgently returned to theatre for treatment of recurrent disease. On that occasion, an ileostomy was fashioned. At the time of surgery, the bypassed region of intestine was examined and found to contain only ‘burned out ileitis (22)’. It was recognized that cancer could develop in the bypassed region and disease recurrence rates of up to 80% prevailed (19,23-26). As a result, intestinal resection substituted bypass as the standard surgical treatment of Crohn’s disease.
Intestinal resection
Radical and conservative intestinal resection were compared. In 1971, Krause et al. demonstrated benefits with radical resection but these findings were not replicated on a large scale (23,27-30). Given the risk of short bowel syndrome and intestinal failure associated with repeated resection, research focused on mechanisms of conserving intestine. Investigation turned towards answering the question as to whether a negative resection margin (i.e., margin free of inflammation) was required in Crohn’s disease (28,31). Pennington et al. examined microscopic margins and determined if there was a correlation with immediate postoperative anastomotic complications. There were no differences in complication rates between patients with, and those without, positive intestinal margins. This suggested that surgeons could afford to adopt less radical approaches to intestinal resection (32). Conservative intestinal resection became the standard practice and has remained so (33).
Stricturoplasty
Efforts to conserve intestine led to the development of stricturoplasty, where the intestine is opened longitudinally and closed transversely (Heineke-Mikulicz stricturoplasty). In a series of nine patients between 1979 and 1982, Lee and Papaioannou first employed the technique (34). Eight procedures were performed electively and one was performed in an emergency setting. Seven patients had more than one stricture. In the Finney stricturoplasty, closure is alternatively achieved using a side-to-side technique. Stricturoplasty is useful in strictures less than 10 cm in length, although this criterion is challenged with the development more recent techniques. The indications for stricturoplasty are increasing.
In an alternative form of stricturoplasty diseased intestine is opened longitudinally. The proximal intestine is then “piggy-backed” over distal intestine and anastomosed (thereby widening the lumen). The Michelassi side-to-side isoperistaltic stricturoplasty employs a variation of this approach and was developed in the early 1990s (24,35,36). The technique avoids short gut syndrome in patients with long strictures, in those with proximal disease, and in those with previous resections. However, 26% of patients experience disease recurrence, typically within 5 years (37-39).
The Kono-S procedure
The anti-mesenteric, functional end-to-end anastomosis (i.e., Kono-S procedure) was recently described by Kono. It appears to be associated with reduced levels of postoperative recurrence. In this procedure, diseased intestine is resected between two fires of a stapling device (one distal and one proximal). Of note, the mesentery is retained. The staple lines are then sutured together forming a column. Longitudinal anti-mesenteric enterotomies are formed on either side of the staple-column. A transverse, two-layer closure of the enterotomies is then performed. In this manner a new intestinal channel is created that is circumferentially free of any mesenteric attachment. The Kono-S approach is increasingly gaining in acceptance. In an early cohort study involving 18 patients who underwent the Kono-S procedure, mean postoperative Rutgeert’s endoscopic disease score was 0.7 at 6 months (0–3 range of scoring system) (40). In a two centre study including 187 patients who underwent the procedure, only two recurrences occurred in a 32 month follow up period (41).
Early versus late surgery for Crohn’s disease
Some studies suggest that early versus late introduction of surgical treatment increases remission rates in Crohn’s disease. In a longitudinal study involving over 200 patients, ileocolectomy at time of diagnosis (versus a mean of 54 months post diagnosis) was associated with decreased clinical recurrence within 10 years of surgery (42). In an evaluation of 506 patients, surgery within a year of diagnosis was associated with a decreased risk of reoperation when compared to medical treatment (33). Latella et al. followed 490 patients with Crohn’s disease, 115 of whom were diagnosed at emergency surgery. They noticed those diagnosed at emergency surgery required less medical treatment and were less likely to require further surgery, compared with patients diagnosed prior to undergoing elective surgery (43).
Two studies compared early surgery with medical therapy. In an Australian study of patients with ileocolic or ileal disease, 42 underwent early surgery and 115 underwent initial medical therapy (88% with immunomodulators and 60% with biologic agents). 14% of patients who underwent early surgery required re-operation within 5 years, whilst 31.3% of those who received medical therapy required surgery (44). In a separate study involving 506 patients with Crohn’s disease, 14% required resection within 1 year of diagnosis. Re-operation rates were compared between this cohort and those requiring index surgery at a later point. Results varied depending on the analysis performed. Using Kaplan-Meier and multivariate Cox regression analyses, reoperation rates were lower in the early surgery cohort. However, no difference was found when propensity scoring was used (33). The first prospective trial of top down medical therapy vs early surgery is currently in progress, the Early Surgery Versus Conservative Treatment in Patients With Ileocaecal Crohn’s Disease (ESPRIT) trial (45).
The most recent randomised multicentre trial (the LIR!C trial) focused on surgery vs biologic treatment in medically refractory ileocolic Crohn’s. No difference in quality of life at 12 months was seen. This suggests that the expense and potential side effects of anti-TNF treatment may be avoided with the use of early surgery in this cohort (46).
The mesentery in Crohn’s disease
Mesenteric abnormalities are considered as pathognomonic of Crohn’s disease (47). They were highlighted by Crohn who noticed how the mesentery advanced over adjacent intestine. Mesenteric thickening and fat wrapping of the diseased bowel segment are well-documented findings in Crohn’s disease (48). Macroscopic coupling of mesenteric, mural and mucosal disease is found when resection specimens are longitudinally opened and examined (49). Lee et al. noted that inflammation occurred on the mesenteric side of small bowel during stricturoplasty (24). Increased levels of C reactive protein (CRP), a circulating cytokine associated with disease prognosis, are found in mesenteric but not subcutaneous fat of Crohn’s patients (50). In murine models, infliximab increases mesenteric (but not intestinal) anti-inflammatory IL-10 cytokine release (51). It is suggested that post-operative recurrence, particularly after end-side anastomoses, is affected by anastomotic exposure to outputs from nearby mesenteric lymph nodes (52). Emerging radiologic data suggest that mesenteric processes occur earlier than previously thought. MRI-based studies in patients with Crohn’s disease, demonstrate the presence of mesenteric abnormalities in the absence of endoscopic evidence of mucosal disease (53).
Mesenteric disease manifestations were recently quantitated and found to correlate with the percentage of circulating fibrocytes, as well as with the Crohn’s disease activity index (49). This is an important development as it means that mesenteric disease can be quantitated and correlated with other aspects of Crohn’s disease. When this is done, mesenteric disease activity does not appear to be affected by biologic agents, but is worse in patients who smoke (unpublished results).
The above findings suggest that mesenteric events may be important in the pathobiology of Crohn’s disease. This suggestion is not new. Behr proposed that extra-intestinal events may be more important than previously thought, in this condition, and coined the phrase “Inside-out” in reference to pathological events arising beneath the epithelium and extending towards the mucosal epithelium (54).
Should the mesentery be included in resection for Crohn’s disease?
In 1982, Heald et al. demonstrated that inclusion of the mesentery provided improved oncologic outcomes in patients undergoing surgery for rectal cancer (55). Similarly, mesenteric resection is also now standard for patients undergoing surgery for colon cancer. Many authors suggested a similar approach may prove beneficial in Crohn’s disease. To date however, only two studies have investigated this suggestion. The findings of our group recently suggest that inclusion of the mesentery is associated with reduced rates of surgical recurrence. We noted significantly reduced surgical recurrence rates when the mesentery was included as part of intestinal resection for patients with ileocolic Crohn’s disease (47,49). As part of this study it was also noted that a transition zone arises where the mesentery changes from normal to abnormal. At this zone, mucosal and mural abnormalities develop in tandem. The transition zone may provide an important landmark to direct the surgeon as to where to place the proximal intestinal incision. Finally, the study also noted that advanced mesenteric disease predicted increased surgical recurrence and reduced time to recurrence. Together these findings suggest that the mesentery exerts a net negative effect on the adjacent intestine and that mesenteric-based strategies are likely to provide benefits to patients undergoing surgery for Crohn’s disease.
Other groups have had similar findings in relation to the mesentery and Crohn’s disease. In the past, surgeons advocated a close resection of the rectum in patients undergoing proctectomy for Crohn’s disease. According to this approach, the mesorectum is retained. However, failure of healing of perineal sinuses has prompted resection of the mesorectum and emerging work demonstrates this should also be included when proctectomy is being conducted for Crohn’s disease (but not for ulcerative colitis) (56).
Mesenteric resection versus stricturoplasty versus Kono-S procedure
The question arises as to how three very different procedures can be associated with similar and low rates of surgical recurrence in Crohn’s disease. Many argue that it is difficult to adopt resection of the mesentery, when the mesentery is retained in both stricturoplasty and the Kono-S procedure. However, it is possible to reconcile and explain outcomes of all three approaches by considering the anatomical relationship between the mesentery and contiguous intestine.
For example, in the Kono-S procedure (described above), an intestinal anastomosis is created that is circumferentially free of a mesenteric attachment. This is because the anastomosis involves two anti-mesenteric enterotomies. If the anastomosis is separate from the mesentery, then mesenteric inputs are considerably reduced, if not eradicated, at that locus.
Stricturoplasty greatly alters the shape and circumferential length of the intestine, and in so doing may also alter the net effects of mesenteric inputs. The Heinike-Mickulicz, the simplest form, changes the conformation of the intestine by opening it longitudinally and closing it transversely. The Michelassi stricturoplasty similarly alters the conformation by overlapping and anastomosing two segments of intestine. Most stricturoplasties have similar effects in altering the conformation of the intestine. It is feasible this alteration redistributes cellular and molecular inputs from contiguous mesentery in a manner that leads to mucosal, but not submucosal or mesenteric healing.
From the above, it would appear the mesentery has a net negative effect on contiguous intestine in Crohn’s disease. In keeping with this, mesenteric-based strategies that decrease mesenteric inputs (i.e., resection) may slow postoperative disease progression. Alternatively, techniques that alter and reduce mesenteric inputs (the Kono-S and stricturoplasty) may also alter disease progression enough to reduce postoperative surgical recurrence rates.
The impact of surgical genetics on the surgical management of Crohn’s disease
The development of high resolution cellular and molecular technologies may have considerable implications for the surgical management of Crohn’s disease and should be briefly discussed. In 1975, Sanger and colleagues developed the first methods to sequence DNA (57). Early linkage studies followed, in which DNA sequences in healthy and diseased individuals were compared. In 2001, Ogura et al. identified the first gene association in Crohn’s disease. They identified an association between mutations in the NOD2/CARD15 gene (the protein product of which is involved in the recognition of bacterial lipopolysaccharides) and Crohn’s disease. This association supported a pathobiological link between dysregulated innate immunity and the development of Crohn’s disease (58). Rapid advances in genotyping techniques identified associations between mutations in over 100 genes and Crohn’s disease. The majority of these genes have either a modifying or causative effect on the disease (59).
Studies have now shifted from gene-disease associations to genotype-phenotype (i.e., behavioural) correlations (60). The field of surgical genetics has identified associations between genetic mutations and several behavioural properties with surgical implications. For example, the requirement for re-operation in Crohn’s disease is associated with mutations in the IRGM gene (61). Failure of medical therapy leading to a requirement for surgery, is associated with a tumour necrosis factor (TNF) polymorphism. Interleukin receptor gene polymorphisms are associated with rapid disease progression and early surgery after diagnosis. NOD2/CARD15 mutations are associated with structuring disease leading to impaired intestinal function (60,62-64).
At present genotypic properties are not used in directing the surgical and postoperative treatment of patients with Crohn’s disease. It is likely however that, with advances in this field, this may change considerably in time.
Pharmacotherapeutics and implications for the surgical management of Crohn’s disease
The development and usage of biological agents has had a number of implications for the surgical management of Crohn’s disease and should briefly be discussed. Biologic agents were first shown to achieve and sustain remission in patients with medically refractive Crohn’s disease in 1997 and as part of the ACCCENT 1 and II trials. Usage of biological agents such as monoclonal antibodies to anti-TNF, gained widespread acceptance in the mid 2000’s (65,66). The armament of medical treatments developed rapidly and now includes steroids, 5-aminosalicylates, purine analogues/thiopurines, methotrexate, cyclosporine, TNF antagonists and, most recently, anti-VEGF and anti-integrin monoclonal antibodies (67). Following excisional surgery in Crohn’s disease, anti-TNF based monoclonal antibodies are more successful than placebo in achieving clinical and endoscopic remission rates (particularly in patients with aggressive disease) (62-77). However, these promising findings are offset somewhat by the fact that less than 40% of patients retain the same level of benefit after approximately 1 year (78). As a result, re-operation rates have not decreased (79,80). There is a suggestion that rates of emergency resections are declining (which could be attributable to biologic usage) whilst rates of elective resection are increasing in tandem (81,82).
In summary, biologic agents (including emerging biologic agents) seem to temporize and delay the requirement for surgery. Increasing data supports their early implementation in the adjuvant (i.e., postoperative) setting when they may slow disease progression and thereby delay or reduce the requirement for re-operation.
In summary: the position and role of surgery in the management of Crohn’s disease
Previously, surgery was reserved for the management of refractory symptoms or the development of complications. This is now being challenged with increasing data supporting earlier introduction of surgical treatment in Crohn’s disease. Randomised controlled trials are required to determine whether earlier introduction of surgery is beneficial. Such trials should ideally concentrate on homogenous cohorts and outcome parameters should be assessed in a standardized manner.
The role of the mesentery needs to be further investigated and randomized controlled trials are currently underway to determine whether inclusion of the mesentery will indeed be associated with improved outcomes. Given recent findings any such trial should be rigorously standardized in terms of the surgical approach. In keeping with this, proximal intestinal incisions should be placed proximal to the mesenteric transition zone, and whilst the mesentery should be included, the pancreatic root region should be avoided.
Finally, data indicates that molecular techniques reliant on genetic profiling may aid in tailoring surgical approaches. In addition, the early application of biologic or emerging agents in the adjuvant setting may further help in reducing postoperative recurrence.
In summary, the role and position of surgery in the management of Crohn’s disease is rapidly changing. This review suggests advances may be achieved with: (I) earlier adoption of surgery; (II) modification of surgical techniques to reduce mesenteric-based pathobiological inputs; and (III) early adoption of adjuvant treatment strategies directed by mesenteric and genetic determinants of outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Morgani G. Seat and Causes of Diseases. New York: Hafner Publishing, 1960.
- Wilks S. Morbid appearances in the intestines of Miss Bankes. Med Times Gazette 1859;2:264-5.
- Dalziel TK. Chronic intestitial enteritis. Br Med J 1913;2:1068-70.
- Rubio CA, Orrego A, Nesi G, et al. Frequency of epithelioid granulomas in colonoscopic biopsy specimens from paediatric and adult patients with Crohn's colitis. J Clin Pathol 2007;60:1268-72. [Crossref] [PubMed]
- Crohn BB, Ginzburg L, Oppenheimer GD. Regional ileitis. A pathological and clinical entity. JAMA 1984;251:73-9. [Crossref] [PubMed]
- Mulder DJ, Noble AJ, Justinich CJ, et al. A tale of two diseases: the history of inflammatory bowel disease. J Crohns Colitis 2014;8:341-8. [Crossref] [PubMed]
- Ekbom A. The changing faces of Crohn’s disease and ulcerative colitis. In: Targan S. editor. Inflammatory Bowel Disease: From Bench to Beside. Dordrecht: Kluwer Academic Publishers, 2003:5-20.
- Colp R. A case of nonspecific granuloma of the terminal ileum and the cecum. Surg Clin N Am 1934;14:443-9.
- Wirts W, Lyon BB. The incidence of regional ileitis. Am J Dig Dis 1941;8:246-8. [Crossref]
- Tallroth A. Regional enteritis with special reference to its etiology and pathogenesis. Acta Chir Scand 1943;88:407-32.
- Wells C. Ulcerative colitis and Crohn's disease. Ann R Coll Surg Engl 1952;11:105-20. [Crossref] [PubMed]
- Greenstein AJ, Lachman P, Sachar DB, et al. Perforating and non-perforating indications for repeated operations in Crohn's disease: evidence for two clinical forms. Gut 1988;29:588-92. [Crossref] [PubMed]
- Goligher JC. The long-term results of excisional surgery for primary and recurrent Crohn's disease of the large intestine. Dis Colon Rectum 1985;28:51-5. [Crossref] [PubMed]
- Loftus EV, Schoenfeld P, Sandborn WJ. The epidemiology and natural history of Crohn's disease in population-based patient cohorts from North America: a systematic review. Aliment Pharmacol Ther 2002;16:51-60. [Crossref] [PubMed]
- Trnka YM, Glotzer DJ, Kasdon EJ, et al. The long-term outcome of restorative operation in Crohn's disease: influence of location, prognostic factors and surgical guidelines. Ann Surg 1982;196:345-55. [Crossref] [PubMed]
- Maconi G, Colombo E, Sampietro GM, et al. CARD15 gene variants and risk of reoperation in Crohn's disease patients. Am J Gastroenterol 2009;104:2483-91. [Crossref] [PubMed]
- Fichera A, Lovadina S, Rubin M, et al. Patterns and operative treatment of recurrent Crohn's disease: a prospective longitudinal study. Surgery 2006;140:649-54. [Crossref] [PubMed]
- Kirsner JB. Historical origins of medical and surgical therapy of inflammatory bowel disease. Lancet 1998;352:1303-5. [Crossref] [PubMed]
- Kirsner JB. Historical antecedents of inflammatory bowel disease therapy. Inflamm Bowel Dis 1996;2:91-4. [Crossref] [PubMed]
- Shaffer VO, Wexner SD. Surgical management of Crohn's disease. Langenbecks Arch Surg 2013;398:13-27. [Crossref] [PubMed]
- Heaton LD, Ravdin IS, Blades B, et al. President Eisenhower's Operation for Regional Enteritis: A Footnote to History. Ann Surg 1964;159:661-6. [Crossref] [PubMed]
- Hughes CW, Baugh JH, Mologne LA, Heaton LD. A review of the late General Eisenhower's operations: epilog to a footnote to history. Ann Surg 1971;173:793-9. [Crossref] [PubMed]
- Ellis L, Calhoun P, Kaiser DL, et al. Postoperative recurrence in Crohn's disease. The effect of the initial length of bowel resection and operative procedure. Ann Surg 1984;199:340-7. [Crossref] [PubMed]
- Lee EC, Papaioannou N. Minimal surgery for chronic obstruction in patients with extensive or universal Crohn's disease. Ann R Coll Surg Engl 1982;64:229-33. [PubMed]
- Michelassi F, Testa G, Pomidor WJ, et al. Adenocarcinoma complicating Crohn's disease. Dis Colon Rectum 1993;36:654-61. [Crossref] [PubMed]
- Strong SA. Surgical management of Crohn’s disease. In: Holzheimer RG, Mannick JA. editors. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt, 2001.
- Krause U, Ejerblad S, Bergman L. Crohn's disease. A long-term study of the clinical course in 186 patients. Scand J Gastroenterol 1985;20:516-24. [Crossref] [PubMed]
- Heuman R, Boeryd B, Bolin T, et al. The influence of disease at the margin of resection on the outcome of Crohn's disease. Br J Surg 1983;70:519-21. [Crossref] [PubMed]
- Fazio VW, Marchetti F, Church M, et al. Effect of resection margins on the recurrence of Crohn's disease in the small bowel. A randomized controlled trial. Ann Surg 1996;224:563-71. [Crossref] [PubMed]
- Hamilton SR, Reese J, Pennington L, et al. The role of resection margin frozen section in the surgical management of Crohn's disease. Surg Gynecol Obstet 1985;160:57-62. [PubMed]
- Cooper JC, Williams NS. The influence of microscopic disease at the margin of resection on recurrence rates in Crohn's disease. Ann R Coll Surg Engl 1986;68:23-6. [PubMed]
- Pennington L, Hamilton SR, Bayless TM, et al. Surgical management of Crohn's disease. Influence of disease at margin of resection. Ann Surg 1980;192:311-8. [Crossref] [PubMed]
- Golovics PA, Lakatos L, Nagy A, et al. Is early limited surgery associated with a more benign disease course in Crohn's disease? World J Gastroenterol 2013;19:7701-10. [Crossref] [PubMed]
- Lee EC, Papaioannou N. Minimal surgery for chronic obstruction in patients with extensive or universal Crohn's disease. Ann R Coll Surg Engl 1982;64:229-33. [PubMed]
- Michelassi F, Balestracci T, Chappell R, et al. Primary and recurrent Crohn's disease. Experience with 1379 patients. Ann Surg 1991;214:230-8. [Crossref] [PubMed]
- Seifarth C, Kreis ME, Grone J. Indications and Specific Surgical Techniques in Crohn's Disease. Viszeralmedizin 2015;31:273-9. [PubMed]
- Lewis RT, Maron DJ. Efficacy and complications of surgery for Crohn's disease. Gastroenterol Hepatol 2010;6:587-96. [PubMed]
- de Buck van Overstraeten A, Vermeire S, Vanbeckevoort D, et al. Modified Side-To-Side Isoperistaltic Strictureplasty over the Ileocaecal Valve: An Alternative to Ileocaecal Resection in Extensive Terminal Ileal Crohn's Disease. J Crohns Colitis 2016;10:437-42. [Crossref] [PubMed]
- Campbell L, Ambe R, Weaver J, et al. Comparison of conventional and nonconventional strictureplasties in Crohn's disease: a systematic review and meta-analysis. Dis Colon Rectum 2012;55:714-26. [Crossref] [PubMed]
- Fichera A, Zoccali M, Kono T. Antimesenteric functional end-to-end handsewn (Kono-S) anastomosis. J Gastrointest Surg 2012;16:1412-6. [Crossref] [PubMed]
- Kono T, Fichera A, Maeda K, et al. Kono-S Anastomosis for Surgical Prophylaxis of Anastomotic Recurrence in Crohn's Disease: an International Multicenter Study. J Gastrointest Surg 2016;20:783-90. [Crossref] [PubMed]
- Aratari A PC, Leandro G. Early versus late surgery for ileo-caecal Crohn's disease. Aliment Pharmacol Ther 2007;26:1303-12. [Crossref] [PubMed]
- Latella G, Cocco A, Angelucci E, et al. Clinical course of Crohn's disease first diagnosed at surgery for acute abdomen. Dig Liver Dis 2009;41:269-76. [Crossref] [PubMed]
- An V, Cohen L, Lawrence M, et al. Early surgery in Crohn's disease a benefit in selected cases. World J Gastrointest Surg 2016;8:492-500. [Crossref] [PubMed]
- Early Surgery Versus Conservative Treatment in Patients With Ileocaecal Crohn's Disease (ESPRIT). Available online: https://clinicaltrials.gov/ct2/show/NCT02716454. Accessed 23/3/18.
- Ponsioen CY, de Groof EJ, Eshuis EJ. Laparoscopic ileocaecal resection versus infliximab for terminal ileitis in Crohn's disease: a randomised controlled, open-label, multicentre trial. Lancet Gastroenterol Hepatol 2017;2:785-92. [Crossref] [PubMed]
- Coffey JC, O'Leary DP, Kiernan MG, et al. The mesentery in Crohn's disease: friend or foe? Curr Opin Gastroenterol 2016;32:267-73. [Crossref] [PubMed]
- Connelly TM, Juza RM, Sangster W, et al. Volumetric fat ratio and not body mass index is predictive of ileocolectomy outcomes in Crohn's disease patients. Dig Surg 2014;31:219-24. [Crossref] [PubMed]
- Coffey JC, Kiernan MG, Sahebally SM, et al. Inclusion of the mesentery in ileocolic resection for Crohn's disease is associated with reduced surgical recurrence. J Crohns Colitis 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Peyrin-Biroulet L, Gonzalez F, Dubuquoy L, et al. Mesenteric fat as a source of C reactive protein and as a target for bacterial translocation in Crohn's disease. Gut 2012;6:78-85. [Crossref] [PubMed]
- Clemente TR, Dos Santos AN, Sturaro JN, et al. Infliximab modifies mesenteric adipose tissue alterations and intestinal inflammation in rats with TNBS-induced colitis. Scand J Gastroenterol 2012;47:943-50. [Crossref] [PubMed]
- Cameron JL, Hamilton SR, Coleman J, et al. Patterns of ileal recurrence in Crohn's disease. A prospective randomized study. Ann Surg 1992;215:546-51. [Crossref] [PubMed]
- Desreumaux P, Ernst O, Geboes K, et al. Inflammatory alterations in mesenteric adipose tissue in Crohn's disease. Gastroenterology 1999;117:73-81. [Crossref] [PubMed]
- Behr MA. The path to Crohn's disease: is mucosal pathology a secondary event? Inflamm Bowel Dis 2010;16:896-902. [Crossref] [PubMed]
- Heald RJ, Husband EM, Ryall RDH. The Mesorectum In Rectal-Cancer Surgery - The Clue To Pelvic Recurrence. Br J Surg 1982;69:613-6. [Crossref] [PubMed]
- de Groof J, van Ruler O, Tanis P, et al. P434 Close rectal versus total mesorectal excision in patients with inflammatory bowel disease undergoing proctocolectomy or completion proctectomy. J Crohns Colitis 2016;10:S319.
- Available online: https://www.genome.gov/pages/education/genetictimeline.pdf. National Institute of Health NHGRI. Accessed 23/3/18.
- Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature 2001;411:603-6. [Crossref] [PubMed]
- Koltun WA. The future of surgical management of inflammatory bowel disease. Dis Colon Rectum 2008;51:813-7. [Crossref] [PubMed]
- Dubinsky MC, Kugathasan S, Kwon S, et al. Multidimensional prognostic risk assessment identifies association between IL12B variation and surgery in Crohn's disease. Inflamm Bowel Dis 2013;19:1662-70. [Crossref] [PubMed]
- Parkes M, Barrett JC, Prescott NJ, et al. Sequence variants in the autophagy gene IRGM and multiple other replicating loci contribute to Crohn's disease susceptibility. Nature Genetics 2007;39:830-2. [Crossref] [PubMed]
- Farrell RJ, Murphy A, Long A, et al. High multidrug resistance (P-glycoprotein 170) expression in inflammatory bowel disease patients who fail medical therapy. Gastroenterology 2000;118:279-88. [Crossref] [PubMed]
- Cucchiara S, Latiano A, Palmieri O, et al. Polymorphisms of tumor necrosis factor-alpha but not MDR1 influence response to medical therapy in pediatric-onset inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2007;44:171-9. [Crossref] [PubMed]
- Seiderer J, Brand S, Herrmann KA, et al. Predictive value of the CARD15 variant 1007fs for the diagnosis of intestinal stenoses and the need for surgery in Crohn's disease in clinical practice: results of a prospective study. Inflamm Bowel Dis 2006;12:1114-21. [Crossref] [PubMed]
- Targan SR, Hanauer SB, van Deventer SJH, et al. A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohn's disease. N Engl J Med 1997;337:1029-35. [Crossref] [PubMed]
- Hanauer SB, Feagan BG. Lichtenstein GR at al. Maintenance infliximab for Crohn's disease: the ACCENT I randomised trial. Lancet 2002;359:1541-9. [Crossref] [PubMed]
- Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn's disease. N Engl J Med 2013;369:711-21. [Crossref] [PubMed]
- Sands BE, Blank MA, Patel K, et al. Long-term treatment of rectovaginal fistulas in Crohn's disease: response to infliximab in the ACCENT II Study. Clin Gastroenterol Hepatol 2004;2:912-20. [Crossref] [PubMed]
- Present DH, Rutgeerts P, Targan S, et al. Infliximab for the treatment of fistulas in patients with Crohn's disease. N Engl J Med 1999;340:1398-405. [Crossref] [PubMed]
- Regueiro M, Feagan BG, Zou B, et al. Infliximab Reduces Endoscopic, but Not Clinical, Recurrence of Crohn's Disease After Ileocolonic Resection. Gastroenterology 2016;150:1568-78. [Crossref] [PubMed]
- Hanauer SB, Sandborn WJ, Rutgeerts P, et al. Human anti-tumor necrosis factor monoclonal antibody (adalimumab) in Crohn's disease: the CLASSIC-I trial. Gastroenterology 2006;130:323-32. [Crossref] [PubMed]
- Colombel JF, Sandborn WJ, Rutgeerts P, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn's disease: The CHARM trial. Gastroenterology 2007;132:52-65. [Crossref] [PubMed]
- Colombel JF, Schwartz DA, Sandborn WJ, et al. Adalimumab for the treatment of fistulas in patients with Crohn's disease. Gut 2009;58:940-8. [Crossref] [PubMed]
- Sandborn WJ, Feagan BG, Stoinov S, et al. Certolizumab pegol for the treatment of Crohn's disease. N Engl J Med 2007;357:228-38. [Crossref] [PubMed]
- Costa J, Magro F, Caldeira D, et al. Infliximab reduces hospitalizations and surgery interventions in patients with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis 2013;19:2098-110. [Crossref] [PubMed]
- Domenech E, Zabana Y, Garcia-Planella E, et al. Clinical outcome of newly diagnosed Crohn's disease: a comparative, retrospective study before and after infliximab availability. Aliment Pharmacol Ther 2010;31:233-9. [PubMed]
- Regueiro M, Schraut W, Baidoo L, et al. Infliximab prevents Crohn's disease recurrence after ileal resection. Gastroenterology 2009;136:441-50. [Crossref] [PubMed]
- Moss AC, Kim KJ, Fernandez-Becker N, et al. Impact of concomitant immunomodulator use on long-term outcomes in patients receiving scheduled maintenance infliximab. Dig Dis Sci 2010;55:1413-20. [Crossref] [PubMed]
- Sands BE, Anderson FH, Bernstein CN, et al. Infliximab maintenance therapy for fistulizing Crohn's disease. N Engl J Med 2004;350:876-85. [Crossref] [PubMed]
- Lazarev M, Ullman T, Schraut WH, et al. Small bowel resection rates in Crohn's disease and the indication for surgery over time: experience from a large tertiary care center. Inflamm Bowel Dis 2010;16:830-5. [Crossref] [PubMed]
- Cosnes J, Nion-Larmurier I, Beaugerie L, et al. Impact of the increasing use of immunosuppressants in Crohn’s disease on the need for intestinal surgery. Gut 2005;54:237-41. [Crossref] [PubMed]
- Ma C, Moran GW, Benchimol EI, et al. Surgical Rates for Crohn's Disease are Decreasing: A Population-Based Time Trend Analysis and Validation Study. Am J Gastroenterol 2017;112:1840-8. [Crossref] [PubMed]
Cite this article as: Connelly TM, Malik Z, Sehgal R, Coffey JC, Peirce C. Should surgical intervention become a primary treatment modality in Crohn’s disease?—A review of the role of surgery and emerging surgical techniques. Mesentery Peritoneum 2018;2:2.