
Evaluation of the outcome of “telephone clinic” in the follow-up of surgical patients: innovative use of technology for the convenience and improvement of service for patients
Introduction
Surgical outpatient services comprise of new and follow-up patient appointments. Each outpatient clinic comprises roughly of around 30% new and 70% return patients (1) Historically every patient is seen for a personal consultation post-operatively even when the recovery is smooth and for follow-up of the patients. Patients are made to wait often in very confined spaces for prolonged period to have a brief consultation. Although it provides reassurance to the patient and perhaps satisfaction to the operating surgeon, it comes at a cost. The presence of an excessive number of such postoperative patients limits the capacity to see new referrals and progressively adds to the lead time in new referrals being seen.
To change what has become custom and practice in a system can often be a challenge. The concept of deviating from a face-to-face consultation to one based upon available technology is a paradigm change in traditional clinical practice. Technology continues to evolve and innovate at a dazzling pace. It is vital that we use it for the benefit of our patients where appropriate. All European countries have more than 1 phone per person of their population. In Ireland there are 5.7 million phones for a population of 4.5 million (2). Therefore, it seems that the humble telephone is an integral source of communication with our patients. Therefore, contacting patients by phone instead of bringing them to the hospital for verbal conversation seems like a reasonable idea.
In a similar endeavour, the concept of admitting every patient a day pre-operatively (3) which was the norm of surgical practice two decades ago has slowly altered in most hospitals. It is now replaced by day case surgery in specific patient groups and day of surgery admissions even for major cases thereby changing how we can deliver surgery in a more efficient and cost-effective manner. Patients are pre-assessed by phone consultation; follow-up nurse lead specialist interaction is undertaken over the phone and liaison with primary health services conducted in a similar fashion. have improved a great deal along with the understanding of health and health related issues among the public. With the ever-increasing access to internet-based information and the development of an ever-increasing connected world it would seem intuitive that we utilise the humble telephone to introduce a system that would decrease pressure on secondary and tertiary care centres. This not only will make these centres more productive but will make sure that patients in need are taken of in an efficient and prompt manner.
With the tsunami of an ever-increasing waiting list for surgical outpatients, we introduced a new concept of a virtual or telephone clinic nearly 5 years ago for the routine follow-up of surgical patients. It has not only reduced the waiting lists but also reduced the need of patients to visit hospital personally and reduce the cost to hospital and patient as well. Previously patients had to wait hours before being seen by doctor, while all they often needed was a verbal reassurance and interaction to inform the clinician that they are doing well (4). We wanted to assess the success and functionality of our virtual clinic. We collected data for last 3 years of patients who were booked for the virtual clinic and analysed the data. We assessed the viability of a running a virtual clinic and tried to identify subgroups of patients where the virtual clinic was the most successful. Aim of the study is to evaluate the effectiveness of tele clinic and find out sub groups of patients who are more likely not to attend so targeted approach for improvement can be used. We present the following article in accordance with the STROBE reporting checklist (available at https://map.amegroups.com/article/view/10.21037/map-21-1/rc).
Methods
Inclusion and exclusion criteria
After any procedure the patient is assessed for the suitability of telephone clinic by the treating clinician. Patients with language barrier, hearing disorder, major surgical procedures and learning difficulties are excluded. Patients are booked for the telephone clinic after confirming their phone number like normal office-based clinic and they receive an official appointment with date and time of the phone call.
Procedure
On the date of clinic, clinician gets the list of patients on telephone clinic with time of appointment and the patient records in a clinic room with telephone and computer to access patient records. Clinicians call the patient on telephone number provided by the patient and after confirming name, date of birth and address discuss the clinical condition or give the results of test.
Data collection
This is a retrospective observational study analysing a prospectively maintained database using the Hospital In-Patient Enquiry (HIPE) reporting system. Characteristics of the first 1,000 patients who were given appointments for the telephone clinic from January 2015 were analysed. Information about gender, age and type of procedure were collected. The outcomes of interest which were recorded includes attendance, discharged, or need to be rebooked for repeat office-based clinic.
Statistical analysis
SPSS version 24 (IBM corporation USA licenced 1989, 2015) was used for statistical analysis of collected data. Chi-squared and Student’s t-test were done to evaluate correlation of demographics with outcomes.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Committee of St James and Tallaght [REC: 2020-06 Chairman’s Action {15}] and informed consent was not required as anonymised data were collected.
Results
The first 1,000 patients who were given appointment from January 2015 were included. The mean and median age of the patients in the study was 50.6 and 50.0 years respectively. The youngest patient included was 17 and eldest was 89 years old. Distribution can be seen in Table 1, while the flowchart of patients followed up in the clinic is shown in Figure 1.
Table 1
| Division of patients | Variables | Yes | No | P value |
|---|---|---|---|---|
| Attended clinic | Male | 404 | 73 | 0.51 |
| Female | 435 | 88 | ||
| Upto 60 years | 553 | 128 | 0.001* | |
| Above 60 years | 286 | 33 | ||
| Millennial | 250 | 62 | 0.029* | |
| Not a millennial | 589 | 99 | ||
| Discharge after 1st appointment | Male | 287 | 190 | 0.60 |
| Female | 323 | 200 | ||
| Upto 60 years | 421 | 260 | 0.43 | |
| Above 60 years | 189 | 130 | ||
| Millennial | 213 | 99 | 0.002* | |
| Not a millennial | 397 | 291 |
*, represent statistically significant relation.
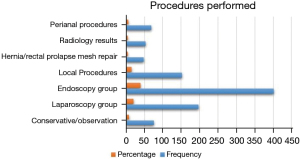
The largest group of patients was of 402 which included patients who were given an appointment in order to outline results of histology of their endoscopic findings. This was either to give results of histology of benign appearing pathologies or assessing outcome following banding or injection sclerotherapy for haemorrhoids. This cohort constituted 40.2% patients. The remaining patients were those that had undergone a laparoscopic procedure. These included laparoscopic appendectomy, laparoscopic cholecystectomy, laparoscopic herniorrhaphy, laparoscopic adhesiolysis and diagnostic laparoscopy (198 patients). The final group of patients had local excision of skin lesions and included patients with excision of local lesions, incision & drainage of abscesses and pilonidal excision respectively (153 patients). This distribution of patients among groups can be seen in Figure 2.
Nine hundred and forty (94%) patients, after receiving appointment, were reviewed via a phone call while 60 (6%) patients in total, mis-interpreted the appointment instructions and showed up in person. These outliners were reviewed as normal in an office-based clinic; 839 (83.9%) patients attended the clinic, while 161 (16.1%) failed to attend or did not receive the phone call; 610 (61.0%) patients out of 1,000 were discharged after the first appointment while 390 (39.0%) were given a second appointment or were booked for office-based clinic. When we exclude the 16.1% patients who did not receive the phone call, 600 (71.5%) of 839 patients were discharged after their telephone consultation. There were 477 males and 523 females comprising 47.7% and 52.3% patients respectively. This can be seen in Figure 3.
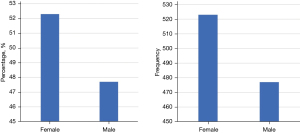
Further analysis was done to identify if there was any relationship between non-attenders and those that were discharged after consultation using the available dataset variables. Gender does not seem to play any role in attendance as Chi-squared test showed no significant difference between males and female attending the clinic (P=0.51). Gender was not related to the possibility of being discharged after the first clinic appointment as no significant relation was with Chi-squared test between gender and discharge (P=0.606). All the statistics is explained in Table 2 as below.
Table 2
| Values | Results |
|---|---|
| Number of patients | 1,000 |
| Age, years | |
| Mean ± SD | 50.6±17.39 |
| Median [range] | 50.0 [17–89] |
SD, standard deviation.
Analysis was performed to find if there was a relationship between age and nonattendance. Student’s t-test found that there was a relation between age and nonattendance. A younger age profile has a significant relationship with nonattendance at the clinic (P=0.0002). There was also a statistically significant relation with younger age and possibility of discharge after first telephone clinic (Student’s t-test P=0.02).
The patients were subdivided into groups depending on their age. This was to ascertain the age group with highest possibility of being discharged from clinic and higher attendance of clinic appointments attendance. Analysis showed that there was no statistically significant difference by Chi-squared test between discharge among patients above or below 60-year age (P=0.445). But statistically significant more patients by Chi-squared test attended the telephone clinic above 60-year age than below it (P=0.001). We use 60 years as a marker as it is the age of retirement in most departments. We had this hypothesis that patients below this age will be less likely to attend the clinic and more likely to be discharged but it was rejected.
The second age group which was analysed was of millennials which by definition is the generation which was born after 1980 (5,6). Analysis showed that there was statistically significant relation by Chi-squared test between discharge rates and patients of millennial generation (P=0.002). Statistically significant relation was found between patients of millennial generation and nonattendance to the telephone clinic by Chi-squared test (P=0.03). This was the age group that was identified as the most likely cohort to get discharge after first clinic but least likely to show up to clinic (7). So targeted efforts should be made to make sure that they attend clinic.
Discussion
Telephone clinic which started as a tool in our facilities to provide ease of contact and avoiding travel for patients who have high percentage of success after procedure but also helping in follow-up after an intervention. This tool equipped us to continue providing high quality care during the pandemic of coronavirus disease 2019 (COVID-19) and due to our experience, we hit the ground running and kept providing facilities to our patients.
Twenty first century is the century of technology and communication. The use of technology in the field of medicine has brought a revolution in providing better results, comfort and improvement in patient care (8). Healthcare systems all around the world are under strain due to increase in demand and the spiralling cost of healthcare. These challenges are further complicated due to the reality of an ever-increasing number of aged patients accessing health care on a regular basis (9). There is a constant effort by the healthcare providers to decrease the cost of healthcare without compromising on the quality of care. Sometimes these efforts are also motivated to produce the best result by changing the attitude or concept of population under care. We continually strive to change concepts and practices in medicine in order to improve patient care. These efforts should always be undertaken in cognisance of the available evidence to support such changes.
The introduction of a telephone clinic for follow-up of our surgical patients was an innovative move made by Tallaght University Hospital five years ago. The rationale behind the introduction of the telephone clinic was to cut the cost of health provision, reduce the waiting time and also to facilitate the patients by abolishing the need to physically come to the hospital for a follow-up surgical clinic. Patients felt that telephone follow up was more convenient in terms of travel time. This often meant not having to drive many miles to attend clinic for follow-up and not having to wait around to see the doctor at the hospital (10). We performed a study to analyse outcome of this innovative approach and to evaluate the success and acceptance of change by the general patient population.
Globally telephone clinics have been used successfully for follow up of patients after different interventions. Several studies have been published to manifest the success of such interventions (11-13). One study demonstrated that contacting patients directly using telephone as compared to sending literature and information through the post resulted in 42.7% patients agreeing and consenting for a procedure as compared to 24.1% with postal communication alone (14). In other study, it has proven to be a safe alternative and nurse led telephone follow-up clinics are helping in the reduction of toxicity with chemotherapy and improving satisfaction in colorectal cancer patients (15). We are currently using the provision of the telephone clinic for benign diseases only. Our study revealed a very high 83.9% attendance rate among patients booked for telephone clinic. At initiation of the telephone clinic, hospital administration assessed patient satisfaction using Likert scale and found 90% satisfaction rate. However only 30% of the patients attending the clinic participated in the survey (16). A randomised controlled trial performed in a similar study to compare satisfaction among patients attending a clinic based follow-up to patients who were followed using telephone clinic found no difference in satisfaction rates among two entities (17). Similar results in safety and satisfaction have been reported by multiple other studies (11-13,18).
In a population of 4.5 million, there are more than half a million patients in Ireland waiting to be seen by specialist doctors. Waiting lists are a problem faced all countries with a publicly funded health system, such as Spain, Australia, New Zealand, Canada, the Netherlands, Ireland and the UK (19). Any effort to reduce the waiting time will also have to deal with the problem of nonattendance at the clinics. Any change in the practice of follow-up in clinics should also be assessed for non-attenders. Our study found out that there were 16.1% patients who did not show up at the appointment. A large Irish study found that there were overall 16.8% nonattendance rates in a large group of appointments that was sent out to patients. But on closer review, it was found that 21% of review patients did not show up for their follow up clinic (1,20-22). As have been previously shown by multiple studies, the most common reason for missed appointments is the resolution of symptoms (23,24). These patients are less likely to make an effort to come to hospital but as our study revealed they are more likely to answer the telephone clinic thus a better attendance rate of 83.9% was seen. Other international studies also recorded no show rates of 22.8% to 28.6% thus confirming the effectiveness of this new modality (20,22,25).
Our study is a retrospective study with reliance of results on patient documents and no feed-back from patients whether they appreciate this new way of communication or not. Extreme care has to be taken while contacting patients through phone and have to make sure you are talking to patient by confirming date of birth and address as violations of General Data Protection Regulation (GDPR) could be done by not doing so. Elderly patients and hard at hearing patients could not be included in study due to mode of communication.
Conclusions
Invented by Antonio Meucci [1849] and patented by Alexander Graham Bell over 100 years ago [1876] the humble telephone continues to be an integral part of our lives. In an era of smart phones, Bluetooth and internet it is this relatively simple device that keeps us all interconnected and its usage continues to evolve on a rapid basis. Its effective application has provided the basis a telephone based virtual clinic in our centre for over five years. Telephone clinics are safe, cost-effective, convenient and a patient friendly alternative to conventional clinics. Careful selection of patients is essential for the success of these clinics. Minor procedures, day cases, endoscopy follow-up or histology results and laparoscopic appendicectomies can be followed-up in this clinic. Interestingly our data identifies the “millennials” as the group least likely to attend yet are most likely to benefit most from this system. This cohort is reflective of the current era of interconnectivity and rapid technology assimilation yet need to be targeted to ensure their engagement. Safety, benefit and effectiveness of this technique was brought more to the forefront and used in COVID-19 pandemic, where it resulted in dispensing of health care without increasing risk of transmission of disease.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://map.amegroups.com/article/view/10.21037/map-21-1/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://map.amegroups.com/article/view/10.21037/map-21-1/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Committee of St James and Tallaght [REC: 2020-06 Chairman’s Action {15}] and informed consent was not required as anonymised data were collected.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hogan AM, McCormack O, Traynor O, et al. Potential impact of text message reminders on non-attendance at outpatient clinics. Ir J Med Sci 2008;177:355-8. [Crossref] [PubMed]
- McGuinness S, Bergin A, Keane C, et al. Measuring Contingent Employment in Ireland. ESRI Research Series Number 74; August 2018.
- Concannon ES, Hogan AM, Flood L, et al. Day of surgery admission for the elective surgical in-patient: successful implementation of the Elective Surgery Programme. Ir J Med Sci 2013;182:127-33. [Crossref] [PubMed]
- Miller L, Caton S, Lynch D. Telephone clinic improves quality of follow-up care for chronic bowel disease. Nurs Times 2002;98:36-8.
- Tapscott D. Growing up digital: McGraw-Hill Companies; San Francisco; 1998.
- Prensky M. Digital natives, digital immigrants part 1. On the horizon. 2001;
- Alsop R. The trophy kids grow up: How the millennial generation is shaking up the workplace: John Wiley & Sons; 2008.
- Ruiz Morilla MD, Sans M, Casasa A, et al. Implementing technology in healthcare: insights from physicians. BMC Med Inform Decis Mak 2017;17:92. [Crossref] [PubMed]
- McIntyre D, Chow CK. Waiting Time as an Indicator for Health Services Under Strain: A Narrative Review. Inquiry 2020;57:46958020910305. [Crossref] [PubMed]
- Cox A, Bull E, Cockle-Hearne J, et al. Nurse led telephone follow up in ovarian cancer: a psychosocial perspective. Eur J Oncol Nurs 2008;12:412-7. [Crossref] [PubMed]
- Overend A, Khoo K, Delorme M, et al. Evaluation of a nurse-led telephone follow-up clinic for patients with indolent and chronic hematological malignancies: a pilot study. Can Oncol Nurs J 2008;18:64-73. [Crossref] [PubMed]
- Gethins S, Robinson R, de Caestecker J, Stewart J. Impact of a nurse−led telephone clinic on quality of IBD care. Gastrointestinal Nursing. 2007;5:34-9.
- Sardell S, Sharpe G, Ashley S, et al. Evaluation of a nurse-led telephone clinic in the follow-up of patients with malignant glioma. Clin Oncol (R Coll Radiol) 2000;12:36-41. [Crossref] [PubMed]
- Steffen LE, Boucher KM, Damron BH, et al. Efficacy of a Telehealth Intervention on Colonoscopy Uptake When Cost Is a Barrier: The Family CARE Cluster Randomized Controlled Trial. Cancer Epidemiol Biomarkers Prev 2015;24:1311-8. [Crossref] [PubMed]
- Craven O, Hughes CA, Burton A, et al. Is a nurse-led telephone intervention a viable alternative to nurse-led home care and standard care for patients receiving oral capecitabine? Results from a large prospective audit in patients with colorectal cancer. Eur J Cancer Care (Engl) 2013;22:413-9. [Crossref] [PubMed]
- Oliver-Dussault C, McGovern B, Whelan M, et al. Telephone clinics: an efficient alternative to surgical review out-patient clinics. Irish Journal of Medical Science 2013;182:S47.
- Beaver K, Campbell M, Williamson S, et al. An exploratory randomized controlled trial comparing telephone and hospital follow-up after treatment for colorectal cancer. Colorectal Dis 2012;14:1201-9. [Crossref] [PubMed]
- Turner B, Wells P. Evaluating the efficacy of a telephone follow-up clinic. Cancer Nursing Practice (through 2013) 2012;11:32-5.
- Black N. Surgical waiting lists are inevitable: time to focus on work undertaken. J R Soc Med 2004;97:159-60. [Crossref] [PubMed]
- Low SK, Khoo JK, Tavintharan S, et al. Missed Appointments at a Diabetes Centre: Not a Small Problem. Ann Acad Med Singap 2016;45:1-5.
- Corfield L, Schizas A, Noorani A, et al. Non-attendance at the colorectal clinic: a prospective audit. Ann R Coll Surg Engl 2008;90:377-80. [Crossref] [PubMed]
- Ratmansky M, Hai N, Schlossberg T, et al. Does pain take holidays? Non-attendance rates at a hospital-based pain clinic are elevated during the Jewish high-holidays. Isr J Health Policy Res 2017;6:11. [Crossref] [PubMed]
- Hardy KJ, O'Brien SV, Furlong NJ. Information given to patients before appointments and its effect on non-attendance rate. BMJ 2001;323:1298-300. [Crossref] [PubMed]
- Potamitis T, Chell PB, Jones HS, et al. Non-attendance at ophthalmology outpatient clinics. J R Soc Med 1994;87:591-3. [Crossref] [PubMed]
- Shah SJ, Cronin P, Hong CS, et al. Targeted Reminder Phone Calls to Patients at High Risk of No-Show for Primary Care Appointment: A Randomized Trial. J Gen Intern Med 2016;31:1460-6. [Crossref] [PubMed]
Cite this article as: Bashir Y, Al-Awaysheh MMH, McGovern B, Rahman A, Olanyi J, Skeens J, Cronin T, Neary P. Evaluation of the outcome of “telephone clinic” in the follow-up of surgical patients: innovative use of technology for the convenience and improvement of service for patients. Mesentery Peritoneum 2023;7:2.



